
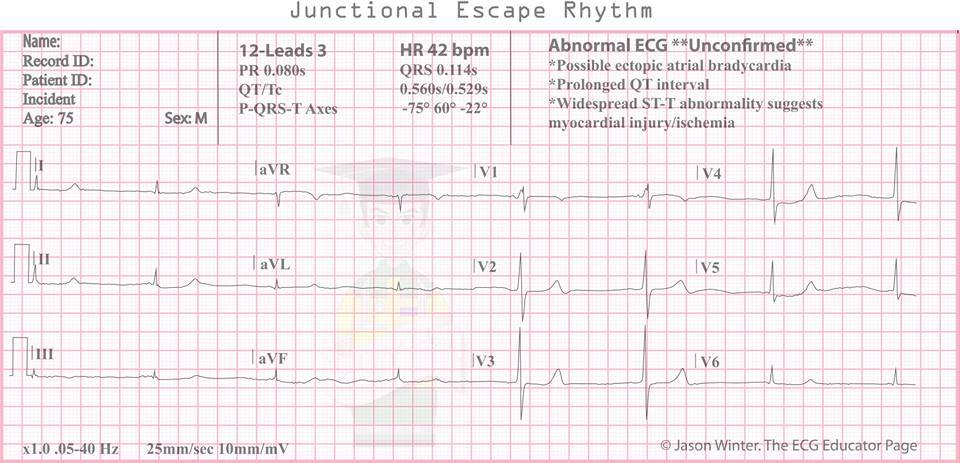
have reported cases of intraoperative junctional rhythms, and epinephrine was suggested to cause imbalances in the pacemaker activities of the sinus and atrioventricular (AV) nodes. Recent evidence suggests that junctional rhythms may be attributed to various mechanisms, all of which involve triggered activity and abnormal automaticity. There were no significant changes in other parameters-such as oxygen saturation, end-tidal CO 2 partial pressure, and peak airway pressure-while the patient exhibited arrhythmias and hypotension. The electrocardiogram showed a normal sinus rhythm around 6 min after the onset of the junctional rhythm ( Fig. The systolic blood pressure increased to 138 mmHg and remained around 110 mmHg when measured at intervals of 2–3 min for 10 min. Two, 8-mg intravenous injections of ephedrine were administered. The patient's noninvasive systolic blood pressure was 50 mmHg immediately after we noticed the changes in the electrocardiogram. At 5 min after the infiltration of lidocaine containing epinephrine, the electrocardiogram revealed an accelerated junctional rhythm, with a heart rate of 70 beats/min ( Fig. All injections were administered after aspiration and completed in around 3–4 min. The inferior alveolar nerve block was performed first, and submucosal infiltration was administered to the depth of the mucobuccal fold and around the lesion.
After induction of anesthesia, the electrocardiogram showed a sinus rhythm with a heart rate of 61 beats/min, and the patient's noninvasive blood pressure was 111/63 mmHg.Īt 20 min after the induction of anesthesia, we administered a local infiltration of 8 mL of 1% lidocaine (10 mg/mL) combined with 1:100,000 epinephrine (10 µg/mL) before the surgical incision. Ventilation was controlled to achieve an end-tidal CO 2 partial pressure of 35–45 mmHg with a mixture of O 2 and air. General anesthesia was maintained with propofol (with a target effect-site concentration of 3–4 µg/mL) and remifentanil (with a target effect-site concentration of 3.5–4.5 ng/mL) to achieve a bispectral index of 40–55. Nasotracheal intubation was performed after administration of intravenous rocuronium (40 mg). General anesthesia was induced with a target-controlled intravenous infusion of propofol and remifentanil. Her blood pressure was 140/78 mmHg and oxygen saturation was 99% on pulse oximetry. An electrocardiogram before the induction of anesthesia showed sinus rhythm with a heart rate of 58 beats/min. The patient received no premedication, and standard monitoring was performed. The day before surgery, her mean blood pressure and pulse rate were 136/71 mmHg and 54 beats/min, respectively. No abnormalities were observed on preoperative chest radiography and routine laboratory examinations.
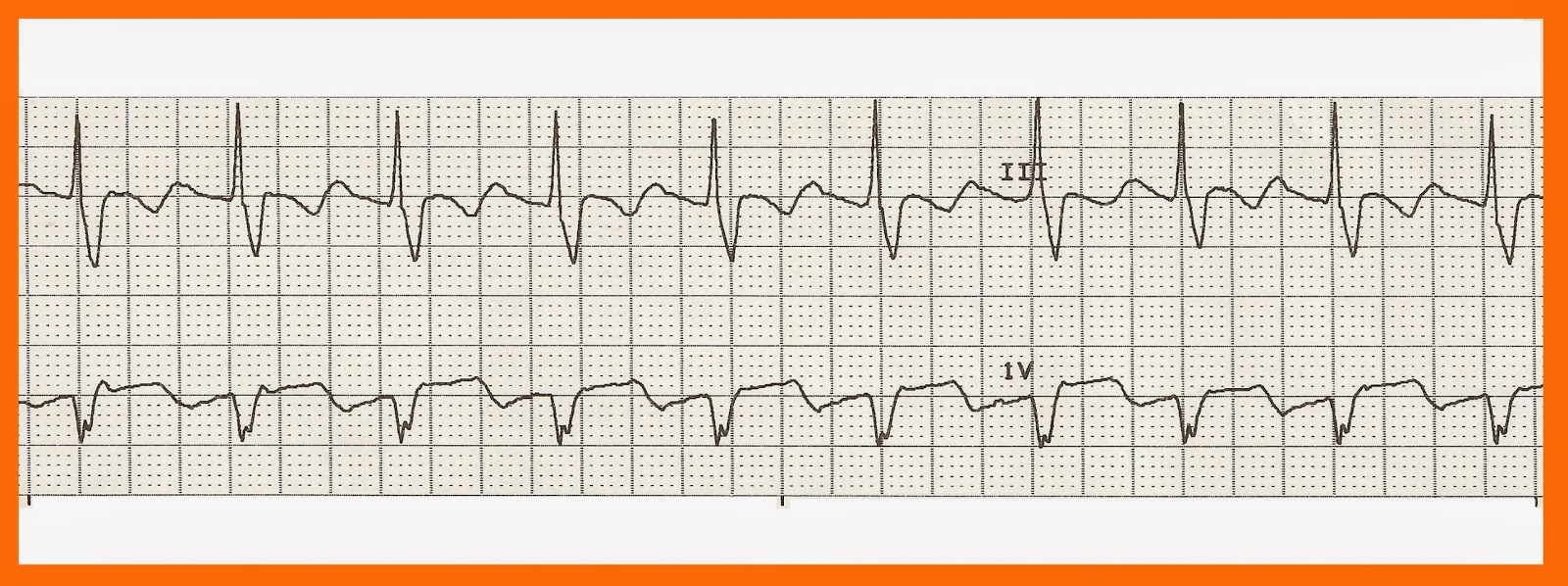
The patient's preoperative electrocardiogram revealed sinus bradycardia with a heart rate of 55 beats/min and no associated clinical symptoms such as dizziness or syncope. She was diagnosed with hypertension and had been taking an angiotensin receptor blocker for 2 years, with no other home medications. In this report, we present our experience with a patient who developed intraoperative junctional rhythm and severe hypotension following regional injection of a local anesthetic that contained epinephrine.Ī 69-year-old woman (height 159 cm weight 55 kg) was scheduled for mandibular dentigerous cystectomy under general anesthesia. Regional infiltration of local anesthetics that contain epinephrine is widely used for pain control and reducing blood loss during surgery however, systemic side effects of this procedure-such as hypertension, tachycardia, and other arrhythmias-have been documented in the literature. Volatile anesthetics can affect the sinoatrial (SA) node and may be associated with the development of junctional rhythm during surgery. An accelerated junctional rhythm usually has a rate between 60 and 100 beats/min and can result from a variety of conditions, including digoxin toxicity, open cardiac surgery, acute myocardial infarction, or isoproterenol infusion. Junctional rhythm is slower than the expected sinus rate. A junctional rhythm is characterized by QRS complexes and is morphologically identical to sinus rhythm, without the preceding sinus P-waves.


 0 kommentar(er)
0 kommentar(er)
